“Most people in Hawke’s Bay have at least one P user in their street,” claims MP Lawrence Yule. No one Bay Buzz interviewed disputes this claim, or even appears shocked – not the police nor the government; not researchers, nor therapists; not recovered addicts, nor community activists.
Measuring illegal drug use is not an exact science. Yule proposes testing wastewater residue to understand the scope of the problem. In October, Police Minister and MP for Napier, Stuart Nash announced that New Zealand Police would be expanding the scheme trialled in parts of Auckland, Whangarei, and Christchurch to cover much of the country, including Hawke’s Bay. Nash hopes that the data gleaned will “allow us to target resources appropriately – both health resources and police resources.”
The New Zealand Health Survey ties Hawke’s Bay with Northland as regions of greatest use. Of the general population, 1.4% admits to using methamphetamine in the past year, compared with 0.8% nationally. This jumps to 2.3% in Hawke’s Bay neighbourhoods with the least deprivation.
Amphetamine Use in Hawke’s Bay by Neighbourhood Deprivation
Quintile (least most deprived)
1 2 3 4 5
2.3% 1.0% 1.2% 1.1% 1.7%
(Source: Ministry of Health New Zealand Health Survey 2014-2017)
Public health research psychologist, Amber Logan, speaks from experience of extensive community consultation, which focused her PhD research on this issue.
“It’s everybody’s problem. It’s our community. Characterising it as a brown people’s problem or a poor people’s problem is just wrong.” She sees users from every section of Hawke’s Bay society, giving this example …
Sid and Nancy (not their real names) own a beautiful home in a desirable suburb. Their garden is manicured; a row of red band gumboots, lined up from large-to-small, at their door. They are small business owners. They pay their taxes. Their cherubic children – clean, cared for, stylishly clothed – beam from photographs across the walls. But they have clawed their way back to middle-class bliss from a nadir of addiction, ill-health and despair. “Corporate munters, we called ourselves…at the beginning I still went to work in a really nice place, dealt with people all day…it gives you the ability to tell yourself you’re fine.”
According to Detective Sergeant Dave de Lange, head of Eastern Police’s Criminal Investigations Bureau, synthesising meth is relatively simple, though dangerous, making methamphetamine the lifestyle drug of choice, over home bake heroin, which previously dominated. Former meth cook turned anti-P activist, Brendon Warne, claims to have extracted the chemical from native plants, some of which do contain ephedrine.
Since banning the active ingredient, ephedrine – a nasal decongestant – ready-made meth, or its component parts, are imported. Although prices are dropping – a gram selling on today’s streets for $500 just a few years ago fetched up to $1,000 – New Zealand is one of the more expensive markets, making import lucrative. On the dark web, a gram can be obtained for as little as US$9 – a profitable mark up, even with customs seizures.
From conversations with community police, Logan concludes, “There are several millions of dollars of meth changing hands every week in Hawke’s Bay.”
Yule favours introduction of the model trialled in Northland – using proceeds of crime to fund more robust and immediate treatment. He and Nash are putting party political differences aside to work across the aisle for change. Nash has visited police in Whangarei and is impressed by their results. “This isn’t about politics…it’s about doing what’s right for our community – investing in social and medical infrastructure that will provide addicts with the outcomes they need, but also to invest in law and order to ensure that we can stop the supply.”
Detective de Lange is mustering assets seizures – trying to make good on the promise crime doesn’t pay. He hopes increased numbers will expand the police’s capacity for prevention, and funnel users into treatment, rather than being the ambulance at the bottom of the cliff. Nash promises that more than a quarter of new police recruits will be focused on organised crime, which he holds responsible for the supply of methamphetamine on our streets.
Your Brain on Meth
Methamphetamine was first given to fighter pilots in World War II as a stimulant to aid focus and wakefulness. It was prescribed for weight loss before negative effects led to criminalisation, though not cessation of use. It can be swallowed, snorted, smoked or injected.
The initial rush creates a surge of dopamine – the happiness hormone – far in excess of other drugs…or sex, gambling, chocolate. Warne, former meth cook who has since become a licensed minister, likens it to a religious experience. “It made me feel like Superman. I thought I was enlightened – I actually got really spiritual.”
This rush subsides to a wakeful high. Middle-class Nancy recalls, “Meth makes you feel like you’re getting a lot done, but you’re just doing fuck all really fast.” As the high drops off, users binge to maintain a buzz that, thanks to tolerance, has diminishing return.
After an extended, often days-long, period without sleep, comes the ‘tweaking’ stage, which Nancy remembers thus: “You’ve got vertigo, you’re confused, you think people are saying things they’re not” – before a crash where users sleep for days.
A period of semi-normalcy can ensue, though this disappears with frequent use. When the brain becomes accustomed to elevated dopamine levels, withdrawal can be excruciating. Logan highlights the risk of suicide at this point, or of beginning the cycle of abuse again. “The dopamine’s burned out – they literally can’t feel good.”
“You want more and more, faster and faster, until you’re a slave to the drug. That’s the nature of the chemical profile of meth – highly addictive, creates tolerance very quickly, very hard to treat.” Logan describes the effects on the brain as analogous to a car whose engine – the impulsive, fight or flight response – is revved up, while the brakes – the higher processing functions allowing rational thought and inhibitory responses – are failing.
Meth also damages the ability to lay down new memories, challenging traditional methods of therapy that support users to form new, more healthy habits. The effect on children in utero is most chilling. These changes occur in the developing brain with profound and permanent cognitive and behavioural consequences.
Guilty victims
Dr Joseph Stone, a clinical psychologist in the field, has first-hand experience, having raised two adoptive sons exposed to methamphetamine in utero. Despite extensive and expensive therapeutic intervention, his elder son’s inability to control violent impulses or to learn from correction led to incarceration. “The first wave of methamphetamine affected babies are now young adults and are hitting the prison system and the adult mental health systems,” he says.
As a clinician, he believes there is widespread misdiagnosis – as ADHD, Oppositional Defiant Disorder, Autism Spectrum Disorders – although he is quick to point out not all such diagnoses can be attributed to maternal methamphetamine use. “A child should be comprehensively evaluated and have a diagnosis respective of their history and symptomology.”
He believes it is in the interest of upper management of health resources to provide diagnoses that can be medicated rather than offering more expensive global support services. “It becomes all about treating the ADHD instead of looking at the trajectory – this kid is not ever truly going to get better.”
Law enforcement and government are invested in a model that separates out ‘innocent’ addicts to be offered treatment, from ‘guilty’ criminals to be punished. But users who become ensnared do not remain innocent for long.
Lack of impulse control combined with an energy surge leads to violence. Methamphetamine has even been implicated in war crimes. Logan believes methamphetamine contributes to violent crime and domestic and child abuse. The insatiable hunger the drug arouses drives crime – theft, manufacture, dealing. From her years of use, Nancy says, “Every heavy meth user is a dealer at some point.”
More money, more problems
Detective Sergeant de Lange believes money is the primary motivator for methamphetamine distribution, and puts the blame on gangs. He dismisses the idea gang leaders are invested in its eradication. “If that’s their policy they’ve got work to do.” Yule agrees, “There’s a whole supply and funding going on … they get it but the money overrides any concerns.” Nash believes gangs have stepped up their game, taking on a clandestine business model that is sophisticated and lucrative. He vows to invest “significant amounts of money, resource and energy into going after these guys who are peddling misery into our communities.”
As leader of Dannevirke’s Black Power chapter, Brendon Warne was a large-scale cook and distributer. “I thought I was helping my bros. They didn’t have any money … I thought I was doing a good thing. I wasn’t.”
He says leaders are averse to the disloyalty meth inspires, and have even begun drug testing. “Gangs don’t control P, once P comes into the gang, P controls the gang. They can make a lot of money but it always crashes – when your members are on it they don’t love your club, they love that stuff, that’s the only thing they love.” Clearly there is a clash between the illusion of power that drug dealing offers, and the reality of running an organisation when members are getting high on their own supply.
User Nancy never resorted to contact with gangs, but had a steady supply of independent manufacturers. One had a big, beautiful house, surrounded by “toys” – the trappings of wealth – but insisted they congregated, sometimes for days, in a dingy garage. To move between rooms, he opened and locked each consecutive door behind him. “He was completely paranoid, but he was right to be. It didn’t help him in the long run – he went to jail in the end, lost everything.”
In Logan’s research population, she sees the allure of fast cash that meth can present. “Imagine a young person who doesn’t feel they have many prospects in life, can’t get a job, maybe dropped out of school, in a disempowered place. Methamphetamine is an opportunity for a young person like that.” It’s an issue Stone comes up against in mandatory counselling for offenders, some of whom are making, though not retaining, big money. “I have nothing to offer a guy like that – what am I going to say, ‘McDonalds is hiring’?”
The ripple effect
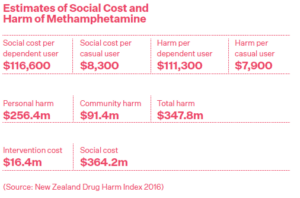
The New Zealand Drug Harm Index estimates the monetary social cost of drug use. It’s a new and complex measure taking into account personal and community harm, petty and organised crime, loss of taxation revenue, policing and court costs, the price of intervention. For addicts, methamphetamine tops the bill with the highest cost per user: $116,600 per annum.
For those without compassion for people locked in the cycle of addiction, Logan hopes this will motivate change. “Surely they can see how much it costs the community … there’s a really good economic reason apart from the social, moral and ethical reasons.”
Logan and Stone come face-to-face with the wide and far-reaching community consequences in their educational talks. Grandparents raising grandchildren, some with profound behavioural problems. Exploitation of family and friends for money. Elder abuse. Vulnerable children exposed to predators while parents crash out. Domestic violence.
Stone likens it to “throwing a rock into a still pool. Trauma spreads through the pool. If you’re in the pool those ripples are going to hit you, even if you don’t get hit by the rock.” Of the users he treats, 95% trace addiction to traumatic wounding. Transmission of trauma through society perpetuates drug abuse in a vicious circle.
Community problem, community solution
Everyone Bay Buzz spoke to spontaneously suggested that holistic engagement from all of us is needed to tackle this problem. Education and awareness are first steps.
Warne founded the Anti-P Ministry, travelling the country, spawning chapters from Whangarei to Otago. His Facebook page, featuring a weekly online church, provides support to thousands. “P took over my life, now fighting P is more important. I want to raise awareness, prevention, education.”
He brings qualities that once made him a gang boss to his activism. Walking down Dannevirke High Street, he is clearly an important community leader. A woman asks to take his photo. Hone Harawira stops to hongi. A dinged-up banger full of patched-up kids throw up their hands in recognition as they hoon past.
The Ministry’s work is funded by merchandise sales – hoodies, t-shirts, hats, stickers – that consciously mimic gang insignia. It makes people look up, show respect. He’s lost some support over his unorthodox methods, over concerns they would prevent efforts to procure funding. “Fuck your funding. We’re doing this because of the people … we’re grassroots.”
His work has brought him into unlikely partnership with local law enforcement who refer users and families to the organisation. A community policeman stops to chat – he’s grateful for the work they’re doing in the town, both as an officer and a citizen. Warne says, “I’ve always had issues with the police but they’ve supported us and helped us achieve – without them we couldn’t have done it.”
The visibility of his movement has made dealers unwelcome in town, as well as educating the community and supporting users to quit. He provides a safe space, food and counselling for users coming off meth. Since getting clean, he earned a qualification in mental health and addiction. “I’m going to do this until my last breath. I’ve got a lot to fix.”
Meth erodes social fabric, sowing distrust in families, in communities. “They’ve usually burned their bridges, but the key is to integrate them back into the community – helping them build trust relationships back with family,” says Logan, adding that an integrated person is much less likely to use, to self-harm, to suffer psychological problems.
For lasting recovery, Logan’s research champions the efficacy of a Family Systems Approach: offering support and education to the “constellation of people and social systems” around the user. Involving them in recovery and placing support structures around them help them to help their loved one. In such cases, “that person will have a much better chance of staying off meth and the family will have a much better chance of being resilient.”
Family ties bring users to treatment. Losing children to CYFS is a primary motivator. “They tend to respond to treatment and get well because they want their kids back,” observes Logan.
For user Nancy, surprise pregnancy led her to recovery. “We were lucky we had a bit of health education, that you don’t do that when you’re pregnant. I understood what that kind of toxic behaviour would do to an unborn child.”
Therapeutic courts, where sentences are suspended on condition of treatment, have been trialled in Auckland and Wellington. From Logan’s academic and Stone’s practical perspectives, they present an opportunity for change. Currently, they see a dearth of wrap-around support and a lack of communication between underfunded, siloed services with long waiting lists. Nash admits, “we really do not have the social and medical infrastructure in place to deal with the methamphetamine epidemic at the moment.”
Logan is invested in educating all sectors of society and community.
“Unless we get community action we’re not going to get change. It takes all of us to recognise the problem and realise it could be our neighbour, our friend,” says Logan. “As long as we keep saying it’s someone else’s problem we’re divorcing it to someone else’s solution. We need a bigger solution than that.”

Blueprint for Change
1. Challenge stereotypes: all sectors of society use, more so in affluent areas.
2. Raise awareness: knowing the signs helps family and friends intervene. Sudden weight loss, unnatural wakefulness followed by long periods of rest, irritability and insolvency are all indicators.
3. Community support: offering help to family and community as well as to users themselves.
4. Wraparound services: communication between services so that when help is sought it can be given, fast.
5. Harm reduction: encourage injectable contraception for users to stem the flow of meth-affected children.
6. Skilled therapy: ensure therapists are educated in the effects of this particular drug rather than applying a generalised treatment model.
7. Follow the money: using asset seizures to fund treatment and to de-incentivise dealing.
8. Therapeutic court: shifting from a judicial model of punishment to one of treatment.

Redemption Song
Chris Jenkins had a sheltered upbringing in a strict Christian household. “I had a lot of rebellion in me”. The family patriarch sought to curb Chris’ rebellious nature with harsh, sometimes physical, discipline. At an up-market Christian boarding school, he dabbled in cigarettes and alcohol. Despite being an accomplished student and athlete, his indiscretions led to exclusion. A ‘normal’ (decile 9) high school first exposed him to drugs. No longer tolerated in the family home, he moved in with an older couple, whose son introduced him to intravenous drug use.
A bender landed him in juvenile court for joyriding and burglary. Treatment for opiate use led him to methamphetamine – the greater high cut through the dampening effect of methadone. He quickly moved into manufacture and distribution – “the money we were making out of meth was unbelievable … we just used it on drugs … I have nothing to show for it.”
Meeting his wife settled him, but their relationship was volatile, even after children. “I would get violent. The marriage was pretty toxic.” He was imprisoned for domestic abuse then bailed to his parents’ house. “I was physically at rock bottom … I lost my job, my family, my freedom … I got out with only the clothes I was wearing when I was arrested.”
A friend introduced him to the twelve step programme. He got sober and attempted to patch up his relationships with his wife and kids, but without addressing his underlying issues his problems persisted. “Drugs weren’t actually the problem – for me they were the solution … abstinence without recovery is a really horrible place to be.”
Despite his history, he was prescribed an opiate-based painkiller for a physical condition, leading him back into the cycle of drug abuse. An ultimatum from his wife sent him to rehab, but he resented his enforced sobriety and the marriage dissolved. “I had no hope … I didn’t care if I lived or died. I was a wreck. Just broken.” The ensuing binge led him to “spiritual rock bottom” from which he re-entered rehab and lasting recovery.
Today, he works with recovering addicts through WIT (Whatever It Takes). “For all the damage I’ve done in society I want to do some positive stuff – to restore balance.” He has not seen his children in five years but is working on mending those relationships, as he has with his father. He now feels compassion for his ex-wife who suffered the worst of his excesses.
A new relationship and new fatherhood has opened his eyes to the capacity for joy that comes with being fully present to one’s own life. After numbing himself for years, he allowed himself to cry for the first time at his grandfather’s funeral – “One last gift from my grandfather, even after he’d died, was that ability to feel stuff … we had a little newborn baby – feeling the feelings that came with that was very special.”

